Antibiotics are medicines used to treat and prevent infections caused by bacteria. They won’t treat illnesses caused by other bugs like viruses. Antibiotics can be life-saving drugs, but many harmful bacteria are becoming resistant to them.
Every year, antibiotics help millions of animals to recover from infections. But they only work against bacteria. And not all bacteria are harmful. Side effects of treatment are common, especially tummy upsets and allergies. If we use antibiotics properly and only when we need them, they’re more likely to work when your cat needs them most.
What it’s for
What are antibiotics used for in cats?
Antibiotics have saved many millions of lives since their discovery by Alexander Fleming in 1928. They’ve increased human life expectancy by 23 years.
Antibiotics are used to kill bacteria.
Bacteria are everywhere, all around us, on us and inside us. We can’t get rid of them all. Most are harmless. Many are good for us.
Bacteria aren’t the only bugs which cause severe illnesses, but antibiotics only work against bacteria.
Antibiotics may be used to treat:
- Severe burns and contaminated wounds
- Dental disease
- Cystitis (bladder infection)
- Blood infections (sepsis)
- Pneumonia (chest infections)
- Bacterial ear infections
- Deep skin infections (pyoderma)
- Complications around pregnancy and birth
- Certain infectious diseases (for example tuberculosis and cat flu)
Antibiotics are used alongside surgery for:
- Dental disease
- Broken bones (orthopaedic surgery)
- Intestinal obstructions or ‘leakage’ (peritonitis)
- Womb infections (pyometra)
Antibiotics are not suitable for:
- Viral infections
- ‘Just in case’ preventives
- Replacing strict hygiene and cleanliness
How it works
How do antibiotics work?
Antibiotics work in two ways:
- Attacking and killing bacteria directly – the bactericidal antibiotics.
- Preventing bacteria from multiplying – the bacteriostatic antibiotics
Bacteria come in many different forms and thrive in different conditions.
- Different types of antibiotics treat different types of bacteria.
- The range of bacteria killed by an antibiotic is called the spectrum.
Broad-spectrum antibiotics kill lots of different types of bacteria.
- Used in many situations where the specific bacteria isn’t identified or more than one is involved.
- Overuse and improper use encourages bacterial resistance
Narrow-spectrum antibiotics are used to target specific types or families of bacteria
- Vets use these where they know the likely bacteria involved or
- After doing a ‘bacterial culture and sensitivity test’ to find out what the bug is and what actually kills it best
- Less risk of longer-term tummy upsets or yeast infections
- More likely to avoid resistance
Commonly used antibiotics in cats
Penicillins ££ and Cephalosporins £££
- Examples: Synulox®, Clamoxyl®, Noroclav®, Cephacare®, Rilexine®
- Bactericidal, broad spectrum
- Destroy bacterial cell walls
- Many uses – bladder, chest, kidney infections, abscesses
Tetracyclines – £- ££
- Examples: Oxycare®, Ronaxan®, Doxybactin ®
- Bacteriostatic, broad spectrum
- Stop bacteria making the proteins they need to grow and replicate
- Mainly used for respiratory infections, urinary tract infections, mycoplasma blood infections (haemobartonellosis) and toxoplasmosis
Potentiated sulphonamides – £
- Examples: Trimacare®, Co-Trimoxazole®, Septra®
- Bactericidal, broad spectrum
- Prevent bacteria making the folic acid they need to survive and multiply
- Bladder, skin, respiratory infections, protozoal diseases
Macrolide Antibiotics – ££
- Examples: Clinacin®, Antirobe®, Zodon®, Clindabactin®
- Bacteriostatic, moderately broad spectrum
- Prevent bacteria from making proteins
- Vets prescribe these antibiotics for skin, dental, chest and bone infections and abscesses.
Fluoroquinolones – £££-££££
- Examples: Marbocyl®, Veraflox®, Baytril®
- Bactericidal, broad spectrum
- These advanced antibiotics prevent bacteria from making RNA and DNA – the very blueprints for the life and workings of a cell
- Fluoroquinolones treat serious and life-threatening illnesses . Their use is limited to serious illnesses or where nothing else works
Metronidazole £-££
- Examples: Metrobactin®, Metrocare®, Stomorgyl®
- Bactericidal, narrow spectrum, but also active against other tiny parasites called protozoa
- Dental, mouth, bladder, gastrointestinal – widely used for it’s additional benefits treating giardia (a protozoan) diarrhoea
Aminoglycosides ££-£££
- Examples: Tiacil® eye drops, Otomax® ear drops, Easotic® ear drops,
- Bactericidal, broad-spectrum
- Prevents bacteria making proteins
- Used in eye drops and ear drops.
- Rarely used ‘inside the body’ because of toxic side effects
Antibiotics will usually start to have an effect within 24 to 48 hours of starting the course. However, for some conditions, it may take much longer to see an improvement. It’s essential to keep giving the medicine as your vet has prescribed.
Antibiotics don’t always cure infections
Antibiotics won’t work if:
- The illness isn’t caused by bacteria
- It’s the wrong antibiotic for the bacteria involved
- The antibiotic can’t get to the site of the infection
- Treatment stops too soon
- Your cat sicks up the medicine before it can work
- The antibiotics aren’t given as prescribed
- The bacteria have become resistant to the antibiotic.
Antibiotic resistance
Antibiotic resistance happens when we overuse antibiotics and use them incorrectly. The massive increase in antibiotic use in the last 50 years has created a huge problem with resistance. Around one million people die every year from antibiotic-resistant infections. It could be any one of us, our family or our cat.
Causes of antibiotic resistance:
- Overusing antibiotics when they’re not needed.
- Not finishing the full course of antibiotic treatment
- Not giving antibiotics as prescribed
- Poor hygiene and cleaning practices
- Overusing antibiotics in farm production
Complications of antibiotic resistance and incorrect use:
- Poorer chance of recovery
- Longer or recurrent illness meaning more vet visits
- Much higher treatment costs
Directions for use
How to give antibiotics to cats
Antibiotics are given as injections, tablets, syrups, capsules drops, creams or ointments.
Only give your cat antibiotics which have been prescribed for them by a vet.
Don’t give human antibiotics to your cat.
- Medicine that helps humans can be poisonous to cats.
- Sometimes vets will treat cats with a human antibiotic or one that’s usually used for other species. This is called ‘off-label’ and will only happen when there’s no cat alternative. Your vet will ask you to sign a consent form for this medicine.
Always give antibiotics at the times and dose your vet prescribed and follow instructions carefully. For example:
- ‘Give with or immediately after food’: The antibiotics may be less likely to cause nausea or vomiting if your cat’s tummy is full and they may be absorbed better.
- ‘Give on an empty stomach’: Give the medicine either an hour before food or 3 hours after feeding. Food in the tummy may interfere with antibiotic absorption.
- ‘Administer whole and do not split or crush’. The medicine may be in a special covering to reduce tummy irritation, disguise a bitter taste, or ensure it’s absorbed at the right part of the intestine.
Useful tips on how to make cats take antibiotics
Warm or strongly smelling food may help to disguise the taste of medication.
If giving tablets directly, always encourage your cat to drink well afterwards by opening a tap or offering flavoured water to drink.
Mix antibiotic powders (from capsules) or tablets with cat pates and offer a small amount where the medication is before offering a full meal.
Side effects
Side effects of antibiotics in cats
All medicines can have side effects. Antibiotics usually target only bacterial cells. However, side effects of treatment are common.
Most adverse reactions to antibiotics happen within the first 24 hours.
The most common side effects include:
- Vomiting
- Diarrhoea: Chronic diarrhoea may continue for weeks after treatment. This happens because antibiotics destroy the friendly bacteria which aid digestion.
- Nausea, drooling and eating less
Cats have a very sensitive throat and oesophagus (the tube taking food to the stomach). Giving tablets with a pill popper tool or by hand can cause oesophagitis (inflammation of the oesophagus) due to irritation from tablets. Tetracyclines, macrolide antibiotics and fluoroquinolones can all cause oesophagitis in cats.
- Allergic reactions: hives and rashes
- Yeast infections: Yeast infections happen with prolonged or repeated antibiotic courses, especially ears and skin. Yeast moves in to take over as both the harmful and the healthy bacteria are killed. Yeast infections can be harder to treat than bacterial infections.
- Blindness and eye damage by certain antibiotics given above recommended dose (Baytril®)
- Seizures and behaviour changes (rare) – metronidazole and fluoroquinolone antibiotics.
How to reduce side effects of antibiotics in cats
- Only getting antibiotics if they’re essential
- Using topical antibiotics rather than giving antibiotics by mouth
- Give tablets with food, unless directed otherwise by your vet to help prevent tablets and capsules getting stuck and damaging the gullet (oesophagus)
- Help your cat’s body to heal with good hygiene and a balanced diet.
- Feed your cat a probiotic: mixtures of friendly bacteria and yeast that can restore a healthy balance and improve gut health. Probiotics can reduce the risk of diarrhoea both during and after antibiotic treatment.
Speak to a vet if :
- You think your cat is having side effects from medication
- You are struggling to give your cat their medicine safely
What happens if
Are antibiotics safe for your cat?
Antibiotics are potent medicines. But sometimes a particular antibiotic won’t be safe for your cat.
Different groups of antibiotics may present risks to different groups of cats. This may mean reducing the dose for some cats or avoiding that antibiotic altogether.
Risks and risk factors associated with certain antibiotics
- Kittens up to 6 months old: tooth discolouration, and interference with bone growth at high doses
- Pregnant cats: harm to unborn kittens, or birth defects
- Allergic reactions: giving the same antibiotic again can cause a much more serious reaction
- Cats with other illnesses may be unable to process and remove antibiotics from the body. This can lead to toxicity, even at otherwise ‘safe‘ doses.
Talk to your vet before starting antibiotic treatment if you think your cat may be in a higher-risk group.
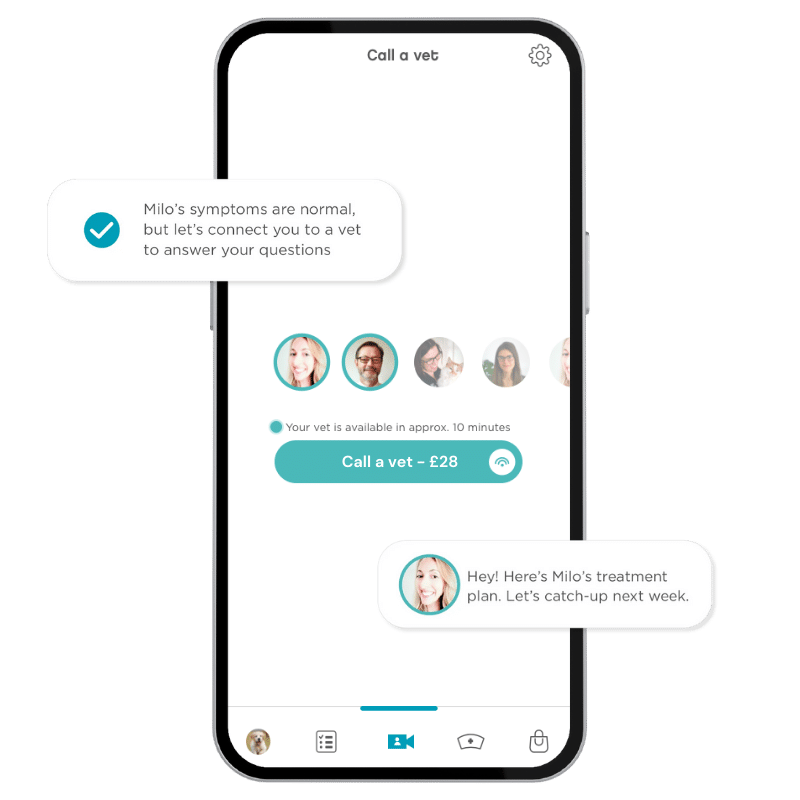
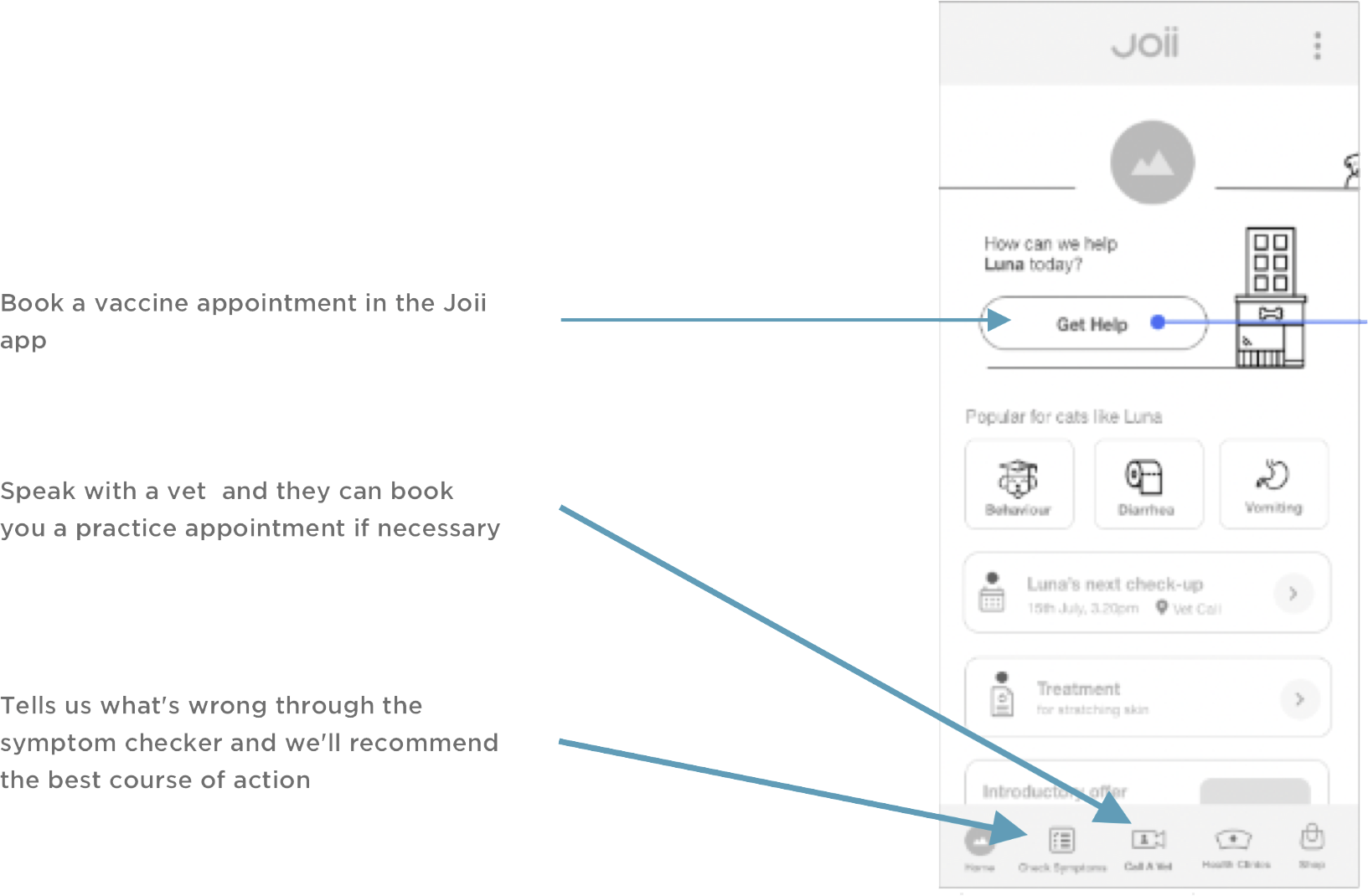
Joii can help with:
- Getting your cat to take medicine
- Recognising and managing side effects of antibiotic treatment
- Understanding if your cat needs antibiotic
- Alternatives to antibiotic treatment where appropriate (especially skin disease)