Mast cell tumours (MCT) are the second most common type of skin cancer in cats. There are forms that can also affect other parts of the body, typically the spleen and intestines. Surgery is the best treatment option when possible, but other treatments can help with the symptoms.
About 20% of skin tumours in cats will be MCT. Disease in the spleen and intestines is less common. MCT on the skin is quite unpredictable, while the other types are usually very serious. All types can also cause allergic-type reactions or stomach ulcers. Milder MCT can often be cured with surgery, but if aggressive or already spread, treatment is difficult and may only work temporarily. Always discuss skin lumps with a vet, especially if there is redness, itchiness or discomfort.
Overview
What are mast cell tumours in cats?
Mast cells are one of the border guards of the immune system. They are in charge of releasing substances that prepare the body to respond when an invader or an injury is detected. Unfortunately, they can suffer mutations and turn cancerous. Two types of mast cell tumours are recognised in cats:
Cutaneous (skin) mast cell tumour
These start as small, hairless skin lumps, usually around the head and neck. Two different forms are recognised.
- Mastocytic type: more common in older cats. About 10% of these will spread aggressively.
- Histiocytic type: more common in younger cats, especially Siamese. There will be multiple lumps but they may disappear spontaneously over time.
Visceral (organ) mast cell tumour
This starts in the internal organs, although some cases will develop metastasis on the skin.
The spleen is affected in more than 85% of cases, with liver and intestinal cases also sometimes seen. This is the most common type of spleen cancer in cats and the third most common intestinal cancer.
Speak to a vet if your pet has a lump that is bothering them or causing redness and swelling of the nearby skin.
Symptoms
Symptoms of mast cell tumours in cats
Cutaneous MCT:
- Lump on or just under the skin, usually around the head and neck.
- Redness and swelling of the skin are common and can develop suddenly.
- The size of the lump may increase suddenly or go through phases of being bigger and then smaller.
- These lumps are often itchy or tender.
- If affecting other organs, symptoms will often involve vomiting, diarrhoea, tarry stools and loss of appetite.
- Allergic-type reactions may involve fainting, weakness, swelling of the face, hives and trouble breathing.
Visceral MCT:
- Lack of energy
- Weight loss
- Vomiting
- Decreased appetite
- Intestinal cases may have diarrhoea and ascites
- Can also develop stomach ulcers and allergic-type reactions
Risk
Cats at higher risk of mast cell tumours
- Most types of mast cell tumours are more common in older cats.
- Histiocytic cutaneous mast cell tumours happen mostly in Siamese cats under 4 years old.
Diagnosis
Diagnosis of mast cell tumours in cats
Mast cell tumours can’t be diagnosed based on their appearance, as this can be unpredictable and may even change over time. Two tests can be done, usually with slightly different goals:
- Fine needle aspirates are done initially to check if a lump is a mast cell tumour or not
- Biopsies will evaluate how aggressive the tumour is likely to be, which helps with treatment decisions
Cases of internal MCT or that have additional symptoms also benefit from:
- Ultrasound scan
- Blood tests
- CT scan
- Biopsy of lymph nodes
- Testing of abdominal fluid, if present
Vet treatment
Vet treatment of mast cell tumours in cats
- Surgery is the best treatment when possible. Ideally, this should be done with wide margins around the visible tumour, as it often extends beyond what can be seen.
- Radiation therapy can be helpful if surgery is not possible or if the biopsy shows there might be tumour cells left after surgery.
- Medications that help with the symptoms or prevent complications may be useful, such as antihistamines and antacids.
Home treatment
Home treatment of mast cell tumours in cats
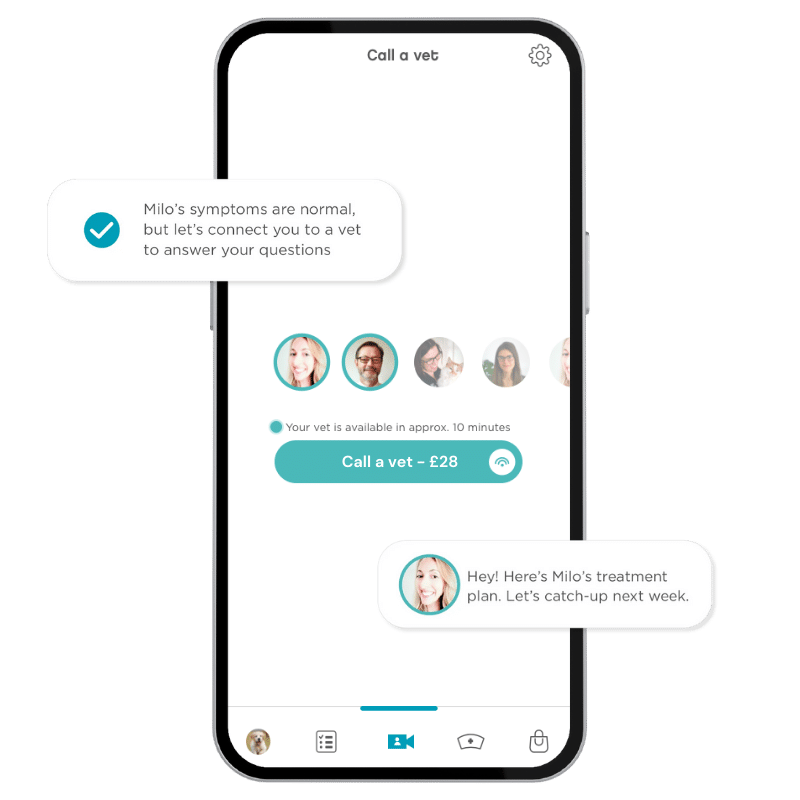
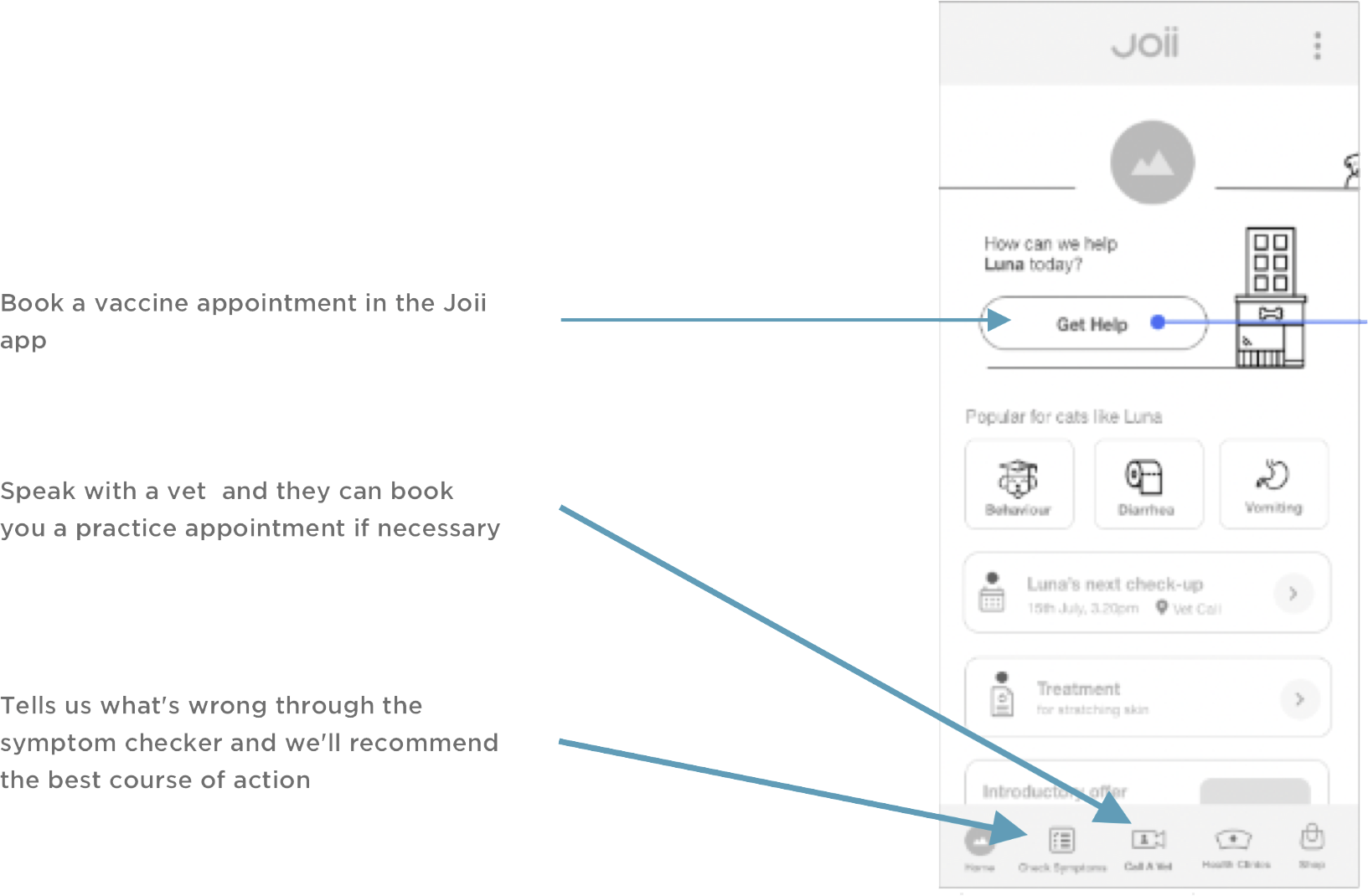
If a lump becomes red, sore or a wound/crust develops, keep the area clean by bathing with saline (1 tsp salt/500ml cooled boiled water) and speak to a vet as soon as possible. Advice is available in the Joii app 24/7.
Living with mast cell tumours in cats
Manipulation or damage to an MCT will increase the risk of pain, digestive complications, and allergic-type reactions. It is important to avoid:
- Self-trauma to the lump (licking or scratching)
- Rough handling of the area
- Hitting or bumping the lump constantly
- If near joints or areas that rub together during movement, rest is advisable
Mast cell tumours can range from a small, slow-growing lump on the skin to malignant cancer. Some will secrete substances with varying effects on the rest of the body. Because of this, every case will be different and have a different prognosis. Spleen or intestinal cases are usually more severe.
Prevention
Prevention of mast cell tumours in cats
Unfortunately, there is nothing specific known to prevent the development of mast cell tumours. A healthy lifestyle, with a balanced diet as well as plenty of exercise, is thought to help prevent all types of cancer.
When to worry
When to worry about a mast cell tumour in your cat
Speak to a vet as soon as possible if your cat has a red or sore skin lump or a lump that is changing in appearance.
If an MCT has been diagnosed, see an emergency vet if your cat:
- Faints or collapses
- Is vomiting a lot, has blood in their vomit or is passing black, tarry stools.
- Develops swelling of the lips or face
- Is struggling to breathe
Speak to a Joii vet as soon as possible if the lump changes in appearance or your cat develops:
- Mild vomiting
- Diarrhoea
- Reduced appetite
- Itching
Advice is available in the Joii app 24/7.