Antibiotics are medicines used to treat and prevent infections caused by bacteria. They won’t treat illnesses caused by other bugs like viruses. Antibiotics can be life-saving drugs, but many harmful bacteria are becoming resistant to them.
Every year, antibiotics help millions of dogs to recover from infections. But they only work against bacteria. And not all bacteria are harmful. Side effects of treatment are common, especially tummy upsets and allergies. If we use antibiotics properly and only when we need them, they’re more likely to work when your dog needs them most.
What it’s for
What are antibiotics used for?
Antibiotics have saved millions of lives since their discovery by Alexander Fleming in 1928. They’ve increased human life expectancy by 23 years.
Antibiotics are used to kill bacteria.
Bacteria are everywhere, all around us, on us and inside us. We can’t get rid of them all. Most are harmless. Many are good for us!
Bacteria aren’t the only bugs which cause severe illnesses, but antibiotics only work against bacteria.
Antibiotics may be used to treat:
- Severe burns and contaminated wounds
- Dental disease
- Cystitis (bladder infection)
- Blood infections (sepsis)
- Pneumonia (chest infections)
- Bacterial ear infections
- Deep skin infections (pyoderma)
- Complications around pregnancy and Birth
- Certain infectious diseases (for example tuberculosis and leptospirosis)
Antibiotics are used alongside surgery for:
- Dental disease
- Broken bones (orthopaedic surgery)
- Intestinal obstructions or ‘leakage’ (peritonitis)
- Womb infections (pyometra)
Antibiotics are not suitable for:
- Viral infections
- ‘Just in case’ preventives
- Replacing strict hygiene and cleanliness
How it works
How do antibiotics work?
Antibiotics work in two ways:
- Attacking and killing bacteria directly – the bactericidal antibiotics.
- Preventing bacteria from multiplying – the bacteriostatic antibiotics.
Bacteria come in many different forms and thrive in different conditions.
- Different types of antibiotics treat different types of bacteria.
- The range of bacteria killed by an antibiotic is called the spectrum.
Broad-spectrum antibiotics kill lots of different types of bacteria.
- Used in many situations where the specific bacteria isn’t identified or more than one is involved.
- Overuse and improper use encourages bacterial resistance
Narrow-spectrum antibiotics are used to target specific types or families of bacteria
- Vets use these where they know the likely bacteria involved, or
- After doing a ‘bacterial culture and sensitivity test’ to find out what the bug is and what actually kills it best.
- Less risk of longer-term tummy upsets or yeast infections.
- More likely to avoid resistance.
Commonly used antibiotics in dogs
Penicillins ££ and Cephalosporins £££
- Examples: Synulox®, Clamoxyl®, Noroclav®, Cephacare®, Rilexine®
- Bactericidal, broad-spectrum
- Destroy bacterial cell walls
- Many uses – bladder, chest, kidney infections, abscesses
Tetracyclines – £- ££
- Examples: Oxycare®, Ronaxan®, Doxybactin ®
- Bacteriostatic, broad-spectrum
- Stop bacteria from making the proteins they need to grow and replicate
- Mainly used for respiratory infections and for leptospirosis
Potentiated sulphonamides – £
- Examples: Trimacare®, Co-Trimoxazole®, Septra®
- Bactericidal, broad spectrum.
- Prevent bacteria making the folic acid they need to survive and multiply.
- Bladder, prostate, anal sac, skin, respiratory infections, protozoal diseases.
Macrolide Antibiotics – ££
- Examples: Clinacin®, Antirobe®, Zodon®, Clindabactin®
- Bacteriostatic, moderately broad spectrum.
- Prevent bacteria from making proteins.
- Vets prescribe these antibiotics for skin, dental, chest anal sac and bone infections, anal sac, bone infections and abscesses.
Fluoroquinolones – £££-££££
- Examples: Marbocyl®, Veraflox®, Baytril®
- Bactericidal, broad spectrum.
- These advanced antibiotics prevent bacteria from making RNA and DNA – the very blueprints for the life and workings of a cell.
- Fluoroquinolones treat serious and life-threatening illnesses. Their use is limited to serious illnesses or where nothing else works.
Metronidazole £-££
- Examples: Metrobactin®, Metrocare®, Stomorgyl®
- Bactericidal, narrow spectrum, but also active against other tiny parasites called protozoa.
- Dental, mouth, bladder, gastrointestinal disease. Widely used for its additional benefits in treating giardia (a protozoan) diarrhoea.
Aminoglycosides ££-£££
- Examples: Tiacil® eye drops, Otomax® ear drops, Easotic® ear drops,
- Bactericidal, broad spectrum.
- Prevents bacteria making proteins.
- Used in eye drops and ear drops.
- Rarely used ‘inside the body’ because of toxic side effects.
How quickly will antibiotics start to work?
Antibiotics will usually start to have an effect within 24 to 48 hours of starting the course. However, for some conditions, it may take much longer to see an improvement. It’s essential to keep giving the medicine as your vet has prescribed.
Antibiotics don’t always cure infections
Antibiotics won’t work if:
- The illness isn’t caused by bacteria
- It’s the wrong antibiotic for the bacteria involved
- The antibiotic can’t get to the site of the infection
- Treatment stops too soon
- Your dog sicks up the medicine before it can work
- The antibiotics aren’t given as prescribed
- The bacteria have become resistant to the antibiotic.
Antibiotic resistance
Antibiotic resistance happens when we overuse antibiotics and use them incorrectly. The massive increase in antibiotic use in the last 50 years has created a huge problem with resistance. Around one million people die every year from antibiotic-resistant infections. It could be any one of us, our family or our dog.
Causes of antibiotic resistance:
- Overusing antibiotics when they’re not needed.
- Not finishing the full course of antibiotic treatment
- Not giving antibiotics as prescribed
- Poor hygiene and cleaning practices
- Overusing antibiotics in farm production
Complications of antibiotic resistance and incorrect use:
- Poorer chance of recovery
- Longer or recurrent illness meaning more vet visits
- Much higher treatment costs
Directions for use
Directions for safe use of antibiotics in dogs
Antibiotics are given as injections, tablets, capsules drops, syrups, creams or ointments.
Only give your dog antibiotics which have been prescribed for them by a vet.
Don’t give human antibiotics to your dog.
- Medicine that helps humans can be poisonous to dogs.
- Sometimes vets will treat dogs with a human antibiotic or one that’s usually used for other species. This is called ‘off-label’ and will only happen when there’s no doggy alternative. Your vet will ask you to sign a consent form for this medicine.
Always give antibiotics at the times and dose your vet prescribes and follow instructions carefully. For example:
- ‘Give with or immediately after food’: The antibiotics may be less likely to cause nausea or vomiting if your dog’s tummy is full and they may be absorbed better.
- ‘Give on an empty stomach’: Give the medicine either an hour before food or 3 hours after feeding. Food in the tummy may interfere with antibiotic absorption.
- ‘Administer whole and do not split or crush’: The medicine may be in a special covering to reduce tummy irritation, to disguise a bitter taste or to make sure it’s absorbed in the right part of the intestine.
Side effects
Side effects of antibiotics in dogs
All medicines can have side effects. Antibiotics usually target only bacterial cells. However, side effects of treatment are common.
The most common side effects of antibiotic treatment include:
- Vomiting and diarrhoea
- Nausea and eating less
- Allergic reactions: hives and rashes
- Yeast infections: Yeast move in to take over as bacteria are killed.
- Dry sticky eyes (potentiated sulphonamide antibiotics)
Most adverse reactions to antibiotics happen within the first 24 hours.
Chronic diarrhoea may continue for weeks after treatment. This happens because antibiotics destroy the friendly bacteria which aid digestion.
Yeast infections happen with prolonged or repeated antibiotic courses, especially to treat ear and skin infections. Yeast moves in to take over as both the harmful and the healthy bacteria are killed. Yeast infections can be harder to treat than bacterial infections.
Tips on how to reduce side effects of antibiotics
- Only getting antibiotics if they’re essential
- Using topical antibiotics rather than antibiotics that go through the whole body
- Helping your dog’s body to heal with good hygiene and a balanced diet.
- Feeding your dog a probiotic
Probiotics contain mixtures of friendly bacteria and yeast that can restore a healthy balance and improve gut health. Probiotics can reduce the risk of diarrhoea both during and after antibiotic treatment.
What happens if
Are antibiotics safe for dogs?
Antibiotics are potent and effective medicines. But sometimes a particular antibiotic won’t be safe for your dog.
Different groups of antibiotics may present risks to different groups of dogs. This may mean reducing the dose for some dogs or avoiding that antibiotic altogether.
Risk and risk factors associated with certain antibiotics:
- Tetracyclines: Puppies up to 6 months old may develop tooth discolouration and interference with bone growth at high doses
- Fluoroquinolones: Growing puppies up to 8 months old, large to giant breeds up to 18 months old might develop joint damage
- Potentiated Sulphonamides: Certain breeds, such as Doberman Pinschers: fever, immune arthritis and life-threatening blood abnormalities
General risks for some groups of dogs
Pregnant bitches:
- Harm to unborn puppies, or
- Birth defects.
- Always tell your vet before starting treatment if you think your bitch may be pregnant.
Dogs with an antibiotic allergy:
- If your dog has had an allergic reaction to an antibiotic, subsequent reactions may be much worse if they get it again.
- Life-threatening anaphylaxis is a risk.
- Make sure your vet knows if your pup has had a previous adverse reaction. Especially if visiting a new vet or unfamiliar practice.
Dogs with other illnesses:
- May be unable to process and remove antibiotics from the body.
- Can lead to toxicity, even at otherwise safe doses.
Talk to your vet before starting antibiotic treatment if you think your dog may be in any higher-risk group.
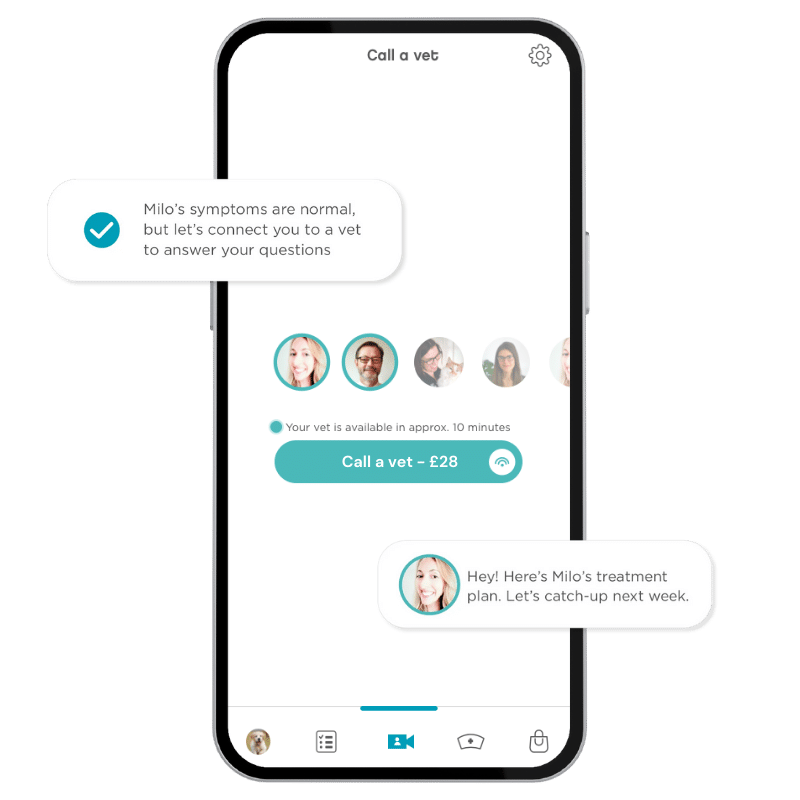
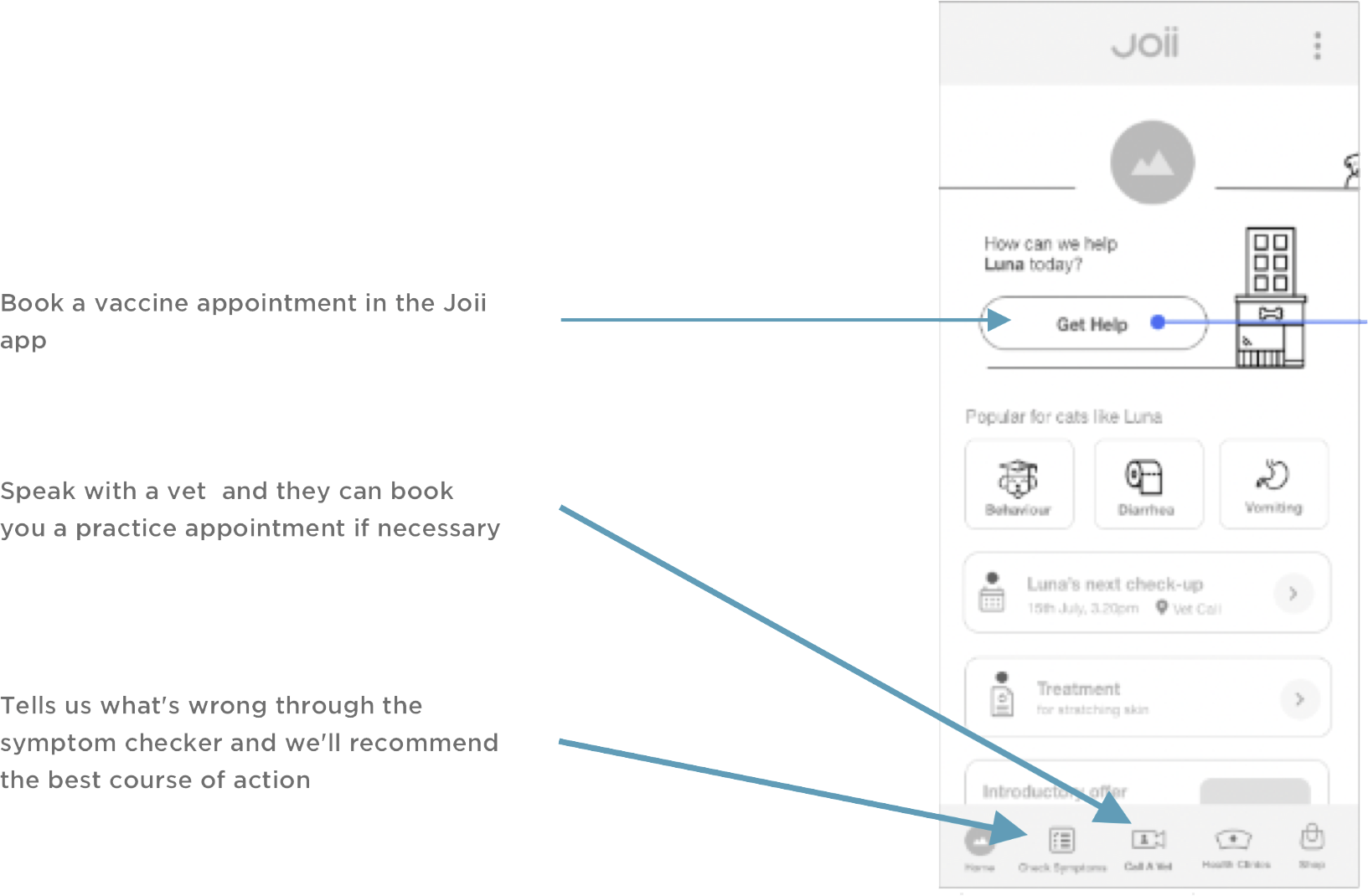
Joii can help with:
- Getting your dog to take medicine
- Recognising and managing side effects of antibiotic treatment
- Does my dog need an antibiotic?
- Alternatives to antibiotic treatment where appropriate (especially skin disease)